Every year, cardiac arrest claims the lives of thousands of people across the world. Prompt and effective cardiopulmonary resuscitation (CPR) is the most critical intervention that can save these lives. Unfortunately, CPR myths and misconceptions abound that could potentially lead to incorrect practices and suboptimal outcomes. In this post, we will bust some of the most common CPR myths and provide evidence-based guidance.
Myth #1: CPR always involves mouth-to-mouth resuscitation, which many people find gross or are uncomfortable performing.
Fact: CPR no longer requires mouth-to-mouth resuscitation in most situations, and chest compressions alone can be highly effective. Chest compressions help pump oxygenated blood to the brain and vital organs, where it will help maintain life until medical help arrives. If you are uncomfortable giving mouth-to-mouth breaths, it’s better to perform hands-only CPR (i.e., continuous chest compressions without rescue breaths) than doing nothing at all.
Myth #2: CPR can restart the heart.
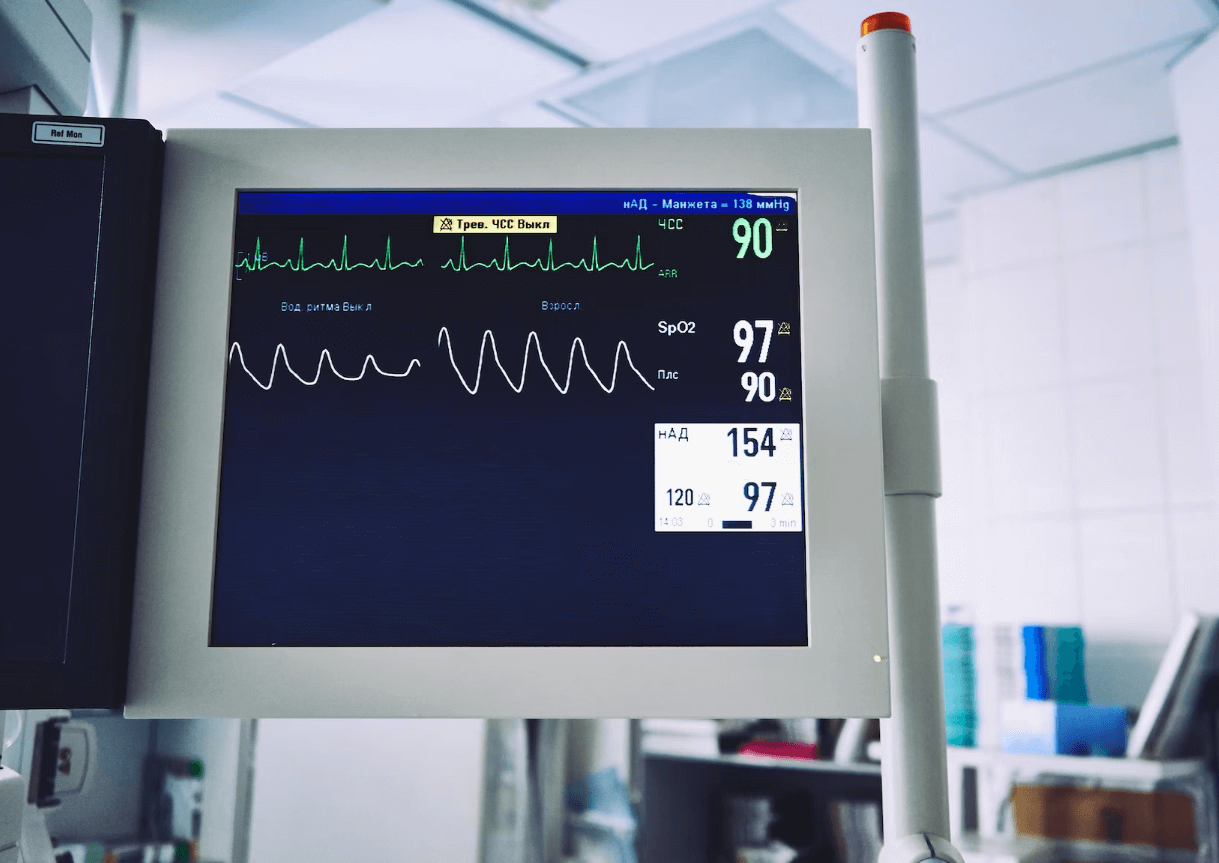
Fact: CPR does not restart the heart, but it buys time for defibrillation. Cardiac arrest often results from an irregular heartbeat called ventricular fibrillation (VF), which can be corrected using defibrillation. Defibrillation uses an electrical shock to restore the heart’s normal rhythm. In contrast, CPR helps circulate the oxygen-rich blood through the body until defibrillation is possible, which is crucial to save a person’s life.
Myth #3: CPR only works in hospitals or emergency rooms.
Fact: CPR is most effective when administered as soon as possible after cardiac arrest. In fact, bystander CPR can double or triple one’s chance of a successful outcome. You don’t have to be a healthcare provider to learn CPR; many organizations offer CPR training, including the American Heart Association, the Red Cross, and local community centers. Learning CPR is also essential for parents, caregivers, and workplace peers.
Myth #4: CPR always causes broken ribs.
Fact: While it is possible to break someone’s ribs during CPR, it’s not a common occurrence. In fact, most people who receive CPR will not have any noticeable injuries. The risk of rib fractures is higher in older adults or those with weaker bones. However, CPR is an acceptable risk because its benefits far outweigh the risks of not performing CPR.
Myth #5: You can’t perform CPR on someone with a pacemaker or an implantable cardioverter-defibrillator (ICD).
Fact: It’s safe to perform CPR on someone with a pacemaker or an ICD, as these devices shouldn’t interrupt chest compressions or rescue breaths. However, avoid placing the defibrillator pads over the pacemaker or ICD as this might cause device malfunction. If you are unsure whether the person has a pacemaker or ICD, follow the standard CPR guidelines.
Knowing the facts and myths surrounding CPR can mean the difference between life and death. Educating yourself on proper CPR techniques and debunking common misconceptions is crucial in improving the cardiac arrest survival rate. Remember, every second counts during cardiac arrest, and the sooner you start CPR, the better the outcome. By busting common CPR myths, we hope to motivate more people to learn this essential life-saving skill and overcome their fears.